Carcinoma of the Breast
Author Lisa Wiechmann MD

History
The Smith Surgical Papyrus from was the first document to ever describe breast cancer.In 1862 Sir Edwin Smith discovered a 4.68 meter long papyrus from 1600 B.C (thought to be a transcript from an older document- 3000 B.C.) and this represents the oldest record on breast cancer. The description included common clinical findings encountered on routine examination in patients with breast cancer and referred to a carcinoma found in a man (case # 45 of 48). The Papyrus proceeds to describing 8 cases of tumors or ulcers of the breast that were treated with a tool called ” the fire drill” similar to the cautery. The conclusion of the text states “there is no treatment” for breast cancer. The document was thought to be written by Imhothep who was later proclaimed God.
Hippocrates ( 460-370 BC) described lesions that affected the breast (distinguished benign and malignant disease), the skin, the stomach, the rectum and the cervix, and classified them. Aulus Cornelius Celsus (25 BC-50AC) described the different stages of evolution of the disease: Cacoethes (early stage) was followed by a carcinoma without ulcer and then by an exophytic lesion. He realized the value of surgery in the early stages of cancer and that only small tumors could be removed whereas “the rest are irritated by every method of cure. The more violent the operations are, the more angry they grow”. ( De Medicina)
Leonidus of Alexandria (180 AC) described breast cancer surgery for the first century after Christ. The procedure included removal of the cancer and of some skin (and healthy tissue). Galen (130-201 AC) believed melancholia and evil humors ( black bile) were the chief factor in the pathogenesis of breast cancer and his treatment consisted of purges, special diets and exorcism. In the second century, Galen inscribed his clinical observation: ” We have often seen in the breast a tumor exactly resembling the animal the crab. Just as the crab has legs on both sides of the body, so in this disease the veins extending out from the unnatural growth take the shape of the crab’s legs. We have often cured this disease in its early stages, but after it has reached a large size, noone has cured it. In all operations we attempt to excise the tumor in a circle where it borders on healthy tissue”. Theories consistent with galenic practice predominated until the Renaissance. In the late 1600s Thomas Willis described a tumor as a “disturbance of growth primarily characterized by cells with uncontrolled, non purposeful division. Fabricius Hildanus (1560-1634) from Germany performed axillary dissections in patients with breast cancer and Marco Aurelio Severini (1580-1656) not only described the different benign and malignant tumors, but also in his description of fibro-adenoma, advised its removal because of its potential to degenerate. Johann Schultes (1595-1645) drew the different stages of a mastectomy in his work “Armamentarii Chirurgici”. Thomas Willis (1621-1675) described tumors as “a disturbance of growing primary cells that are substituted by uncontrolled , non purposefully dividing cells.”
During the 17th century cancer was felt to be contagious and therfore patients with cancer were not allowed in hospitals for fear of an epidemic. This led to the birth of dedicated cancer hospitals , the first of which was founded in Reims in 1740( Hopital St-Louis)
Henri Le Dran (1685-1770) first recognized the spread of cancer to regional axillary nodes and recommended that both the tumor and the axillary lymphnodes be excised. He also recognised that lymph nodes with cancer were indicative of a more advanced stage of the disease.
Gian Battista Morgagni(1682-1771) carried out 700 autopsies on patients with breast, stomach, pancreas and rectal cancer and described his findings in his work ” De Sedibus et Causis Morborum”. John Hunter (1728-1793) was the first physician to observe a predisposition to cancer based on genetics, age, and environmental factors. He estimated that the average age at which people developed cancer was 40-60 years and that if a woman was found to have cancer before the age of 40, the cancer was soon lethal. Astly Cooper (1768-1841) was Hunter’s student and described the fibrocystic mastopathy of the breast and Sir James Paget (1841-1899) desbribes the homonymus disease of the breast.
In the 19th century Moore, of the Middlesex Hospital of London, emphasized the importance of removal of axillary lymph nodes ( palpable and non-palpable) together with the complete resection of the breast. In 1894 Halstead and Meyer each independently brought to the attention of the public , the results of their treatment of breast cancer and described the advantages offered by a radical mastectomy ( Ipsilateral breast, Axillary nodes levels I-III, resection of pectoralis major and minor muscles, resection of thoracodorsal and long thoracic nerves. Halstead reported ” early” breast tumors to measure approximately 8x 7 cm in size. Ten year survival approached 34% .
After Wilhelm Roentgen (1845-1923) discovered X-rays in 1895, Sampson Handley stated that ” the principle of using x-rays for treatment of breast cancer is prophylactic against postoperative relapse.” Ther role of x-ray in evaluating and treating breast cancer continued to grow and allowed detection of non-palpable tumors, therefore leading to new surgical therapies (lumpectomies, quadrantectomies).
In 1948 Patey and Dyson of the Middlesex Hospital in london, advocated a modified radical mastectomy for the management of advanced, operable cancer (with removal of pectoralis minor muscle).
It was Madden who described the Modified Radical Mastectomy as we now know it, with preservation of both pectoralis major and minor and lymphadenectomy of levels I-II ( but not III).
Overview
Breast cancer is the leading cause of death in women 40-55 years of age. It represents the second leading cause of cancer death among american women (all ages) following lung cancer. Approximately 1 in 8 (12.5%) american women will be diagnosed with breast cancer during thier lifetime, and the risk of dying from the disease is approximately 3.4%. Breast cancer accounts for approximately 30% of cancers in women. It’s incidence increases rapidly after 40 years of age and after menopause the rate of increase is slower. Furthermore incidence of breast cancer has been steadily increasing over the past 70 years as demonstrated by data from the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER). Part of this increase has been attributed to an increased detection rate related to the use of mammography. Survival rates have also increased steadily for women with local and regional disease and this is probably due to both earlier detection of cancer and improvement in therapies.Risk Factors
Multiple factors appear to be involved in the pathogenesis of breast cancer: these include genetic factors, environmental factors and endocrine factors. Gender is the most important risk factor for the development of breast cancer, which occurs 100 times more frequently in women than in men. This is due to endocrine factors as mentioned above: factors that increase the number of menstrual cycles (exposure to estrogen) such as nulliparity, late pregnancy (after 30 years of age), early menarche and late menopause( > 30 years menstrual time), are associated with an increased risk of breast cancer. Protective factors include moderate levels of exercise, and a longer lactation period. exposure to exogenous estrogens (oral contraceptive pills and hormone replacement therapy if prolonged in their duration- > 10 years) has though data is controversial. Age is an important risk factor for the development of breast cancer ( which translates in years of exposure to estrogen) ( risk of white American woman at 30 years 1:5,900, at 80 years 1:290)

Prior history of breast cancer is a significant risk factor for the development of breast cancer and proliferative breast diseases have now been found to increase the risk of breast cancer slightly 1.5-2 times the risk (papillomas, florid hyperplasia without atypia, sclerosing adenosis), moderately – 4 to 5 times the risk (Atypical ductal and lobular hyperplasia) and severely- 8 to 10 times the risk (lobular carcinoma in situ).
Environmental factors include exposure to ionizing radiation (mantle radiaton therapy for Hodgkin’s lymphoma -75-fold increase in risk, survivors of the atomic bomb) if exposure was before age 30) and potentially obesity (controversial) and alcohol ( no conclusive evidence). In mice a virus called mouse mammary tumor virus (MMTV), transmitted through the mother’s milk, causes breast cancer in suckling mice. No such virus has been identified in humans to this date.
Any family history of breast cancer increases a woman’s risk of breast cancer, especially if found in first degree relatives. Such risk is dependent on the characteristics of the cancer in relatives ( age at presentation, unilateral or bilateral, number of relatives with cancer).
The Jewish Ashkenazi population displays a 10 fold higher frequency of 2 founder mutations (185delAG and 5382insC) therefore screening of such mutations in then above population is indicated.
The interaction of many different risk factors in the initiation of breast cancer has lead to the creation and use of risk-assessment models. This helps predict the risk of management and determine the best course of action. The most frequently used model was designed by Gail in 1970 and incorporates age at menarche, number of breast biopsies, age at first live birth and the number of first degree relatives with breast cancer. It is used to predict the risk of developing breast cancer per decade of life. One of the disadvantages of this model is that it doesn’t take into account age at which a family member was diagnosed and whether the disease occurred in both breasts — early onset and bilateral disease suggesting a BRCA mutation carrier
Classification
Anatomical Sites and Subsites
1. Nipple
2. Central portion
3. Upper-inner quadrant
4. Lower-inner quadrant
5. Upper-outer quadrant
6. Lower-outer quadrant
7. Axillary tail
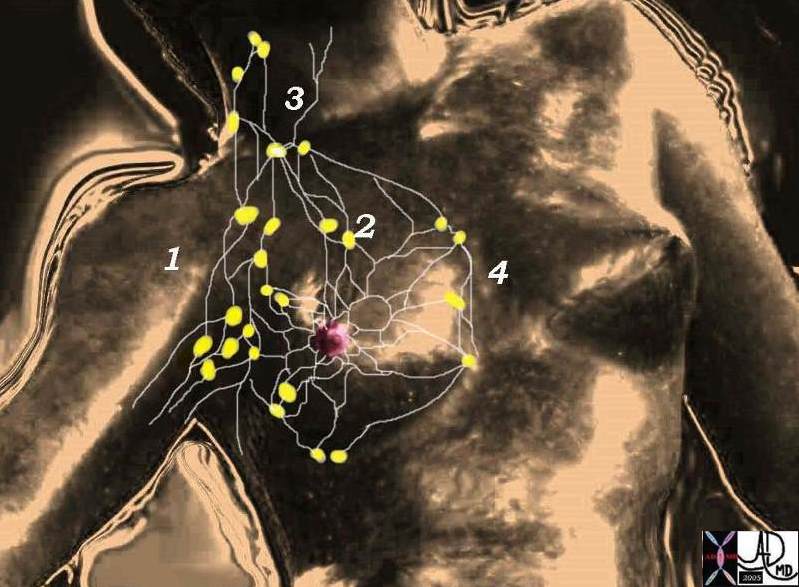
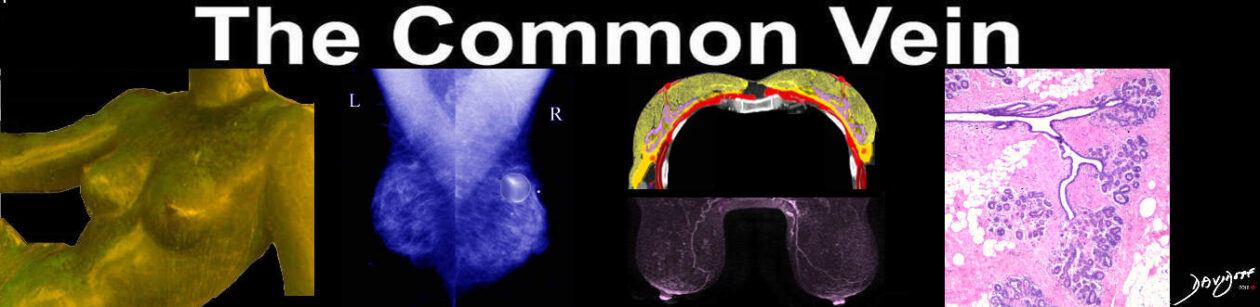
78378pb06l05 breast mammary gland lymphatic drainage lymph nodes axillary lymph nodes infraclavicular lymph nodes supralavicular lymph nodes internal mammary lymph nodes parasternal lymph nodes anatomy normal Courtesy Ashley Davidoff MD
Classification
The regional lymph nodes:
1. Axillary (ipsilateral): interpectoral (Rotter) nodes along the axillary vein and its tributaries, which may be divided into the following levels:
i) Level I (low-axilla): lymph nodes lateral to the lateral border of pectoralis minor muscle
ii) Level Ii (mid-axilla): lymph nodes between the medial and lateral borders of the pectoralis minor muscle and the interpectoral (Rotter) lymph nodes
iii) Level III (apical axilla): lymph nodes medial to the medial margin of the pectoralis minor muscle including those designated as subclavicular, infraclavicular or apical
Note: Intrammamary lymph nodes are coded as axillary lymph nodes.
2. Internal mammary (ipsilateral): lymph nodes in the intercostal spaces along the edge of the sternum in the endothoracic fascia.
Any other lymph node metastasis is coded as distant metastasis (M1), including supraclavicular, cervical, or contralateral internal mammary lymph nodes
Classification – TN Clinical Classification
T – Primary Tumor
TX Primary tumor cannot be assessed
TO No evidence of primary tumor
Tis Carcinoma in situ: intraductal carcinoma, or lobular carcinoma in situ, or Paget disease of
the nipple with no tumor (Fig.3)
Note: Paget disease associated with a tumor is classified according to the size of the
tumor.
T1 Tumor 2 cm or less in greatest dimension (Fig. 4)
Tla 0.5 cm or less in greatest dimension
TIb More than 0.5 cm but not more than 1 cm in greatest dimension
TIc More than I cm but not more than 2 cm in greatest dimension
T2 Tumor more than 2 cm but not more than 5 cm in greatest dimension (Fig. 4)
T3 Tumor more than 5 cm in greatest dimension (Fig. 4)
T4 Tumor of any size with direct extension to chest wall or skin
T4a Extension to chest wall (Fig. 5)
T4b Edema (including peau d’orange), or ulceration of the skin of the breast, or satellite skin
nodules confined to the same breast (Figs. 5, 6)
T4c Both 4a and 4b above (Fig. 6)
T4d Inflammatory carcinoma (Fig. 6)Notes: Inflammatory carcinoma of the breast is characterized by diffuse, brawny induration of the skin with an erysipeloid edge, usually with no underlying palpable mass. If the skin biopsy is negative and there is no localized measurable primary cancer, the T category is pTX when pathologically staging a clinical inflammatory carcinoma (T4d).
Dimpling of the skin, nipple retraction or other skin changes, except those in T4b and 4d, may occur in T1, T2 or T3 without affecting the classification. Note: Chest wall includes ribs, intercostal muscles and serratus anterior muscle but not pectoral muscle.
Classification – N – Regional Lymph Nodes
NX Regional lymph nodes cannot be assessed (e.g. previously removed)
N0 No regional lymph node metastasis
N1 Metastasis to movable ipsilateral axillary node(s) (Fig.7)
N2 Metastasis to ipsilateral axillary node(s) fixed to one another or to other structures (Fig.7)
N3 Metastasis to ipsilateral internal mammary lymph node(s) (Fig.8)
The original source for this material is the AJCC Cancer Staging Manual, Sixth Edition (2002) published by Springer-Verlag New York, Inc.The tumor staging system for breast cancer published by the American Joint Committee on Cancer (AJCC) was modified extensively in 2002. When compared to the classification published in 1997, the major differences are as listed: 1) reclassification of nodal status based on number of positive lymphnodes ( axilla) , differentiation between micrometastases and macrometastases, identifiers to indicate the use of specific techniques ( immunohistochemistry,molecular biology), surgical technique ( sentinel lymphnode biopsy ), and a reclassification of metastasis to internal mammary nodes, and supraclavicular nodes (now designated N3 rather than M1 disease) .These changes have been shown to dramatically affect stage-specific survival.
Classification – pTN Pathological Classification
pT – Primary Tumor
The pathological classification requires the examination of the primary carcinoma with no gross tumor at the margins of resection. A case can be classified pT if there is only microscopic tumor in a margin. The pT categories correspond to the T categories. When classifying pT the tumor size is a measurement of the invasive component. If there is a large in situ component (e.g. 4 cm) and a small invasive component (e.g. 0.5 cm), the tumor is coded pTl a.pN – Regional Lymph Nodes
The pathological classification requires the resection and examination of at least the low axillary lymph nodes (level 1) (see above). Such a resection will ordinarily include six or more lymph nodes.
pNX Regional lymph nodes cannot be assessed (not removed for study or previously removed)
pNO No regional lymph node metastasis
pNI Metastasis to movable ipsilateral axillary node(s)
pN1 a Only micrometastasis (none larger than 0.2 cm) (Fig. 9)
pN I 1b Metastasis to lymph node(s), any larger than 0.2 cm (Fig. 10)
pN1bi Metastasis to one to three lymph nodes, any more than 0.2 cm and all less than 2.0 cm in greatest dimension
pN1bii Metastasis to four or more lymph nodes,any more than 0.2 cm and all less than 2.0 cm in greatest dimension
pN1biii Extension of tumor beyond the capsule of a lymph node metastasis less than 2.0 cm in greatest dimension
pN1biv Metastasis to a lymph node 2.0 cm or more in greatest dimension
pN2 Metastasis to ipsilateral axillary lymph nodes that are fixed to one another or to other structures (Fig. 8, see above)
pN3 Metastasis to ipsilateral internal mammary lymph node(s)
Statistics
Breast cancer accounts for 33% of all female breast cancers and represents the most frequent cause of death in women age 40-45 years. In the 1970s the estimated probability of developing breast cancer for a white American woman was 1:13, in the 1980s it was 1:11 and in 2002 12.5% of women develop breast carcinoma.
Geographic Distribution
The incidence of breast cancer varies significantly among differennt countries, and is highest in Northern European countries and in the United States, intermediate in Southern America and Southern and Eastern Europe, and lowest in Asia (Japan, Singapore and urban China have seen a rise in rates with the advent of Western-style economy). Breast cancer incidence and mortality vary sigificatly within the United States. The incidence of breast cancer appears to be highest in white women from Hawaii (128:100,000) followed by those from San Fransisco and the Northeast.The lowes incidence is found in Utah(98:100,000) and New Mexico
The variation of incidence for African-American woment is relatively small ( 94-106:100,000).
SocieconomicsUnlike most other illnesses a positive correlation has been noted between the lifetime risk of breast cancer and higher socioeconomic status.
Population and age distribution
There is significant variation among different populations in the incidence of breast cancer: as shown below, in the United States the African-American population has a slightly higher risk until the age of forty, after which there is crossover and the highest risk is in the white population.
Patients of Jewish- Ashkenzi-ancestry have a higher risk of developing breast cancer as discussed in the genetics section.
Sex Distribution
M:F < =1:100
Staging of breast cancer
|
Stage
|
Tumor Size
|
Lymph Node Involvement
|
Metastasis (Spread)
|
I
II
III
IV
|
Less than 2 cm
Between 2-5 cm
More than 5 cm
Not applicable
|
No
No or in same side of breast
Yes, on same side of breast
Not applicable
|
No
No
No
Yes
|
Stage
|
Tumor (T)
|
Node (N)
|
Metastasis (M)
|
Stage 0
|
Tis
|
N0
|
M0
|
Stage 1
|
T1
|
N0
|
M0
|
Stage IIA
|
T0
|
N1
|
M0
|
T1
|
N1
|
M0
|
T2
|
N0
|
M0
|
Stage IIB
|
T2
|
N1
|
M0
|
T3
|
N0
|
M0
|
Stage IIIA
|
T0
|
N2
|
M0
|
T1
|
N2
|
M0
|
T2
|
N2
|
M0
|
T3
|
N1, N2
|
M0
|
Stage IIIB
|
T4
|
any N
|
M0
|
any T
|
N3
|
M0
|
Stage IV
|
any T
|
any N
|
M1
|
Source: American Joint Commission on Cancer and International Union Against Cancer
Pathology

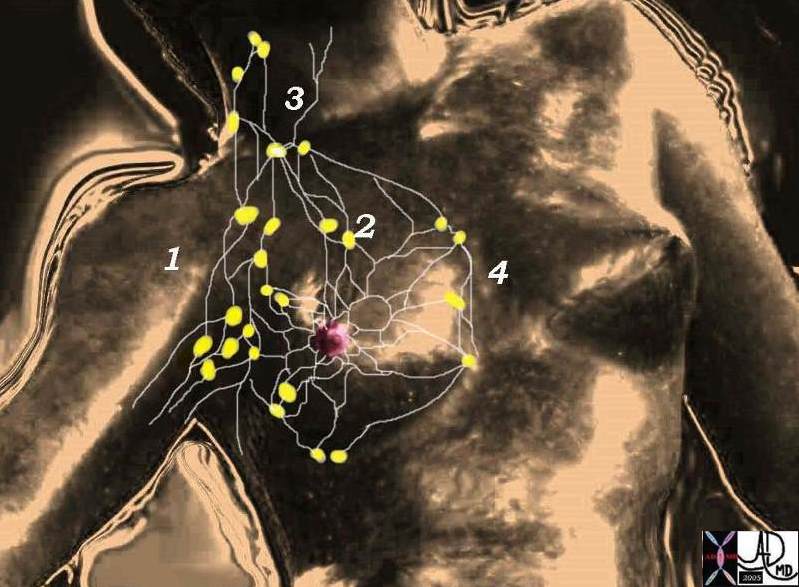
13553 breast + dx infiltrating ductal carcinoma + grosspathology Courtesy Frank Reale MD
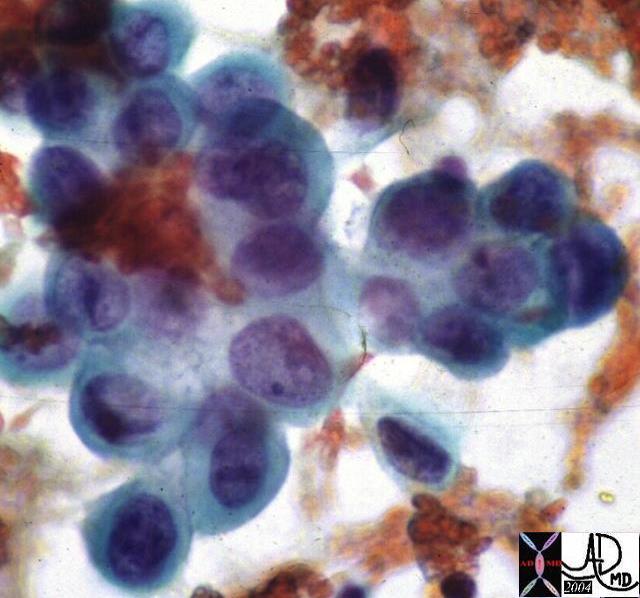
13552 breast + dx infiltrating ductal carcinoma + cytopathology histopathology Courtesy Frank Reale MD DB
Invasive carcinomas of the breast are characterized by histologic heterogeneity. The majority are adenocarcinomas of which 5 variants have been identified:
-
Infiltrating Ductal carcinoma: represents approximately 75-85% of all breast cancers and is characterized by the absence of specific features (NST-no special type). Upon palpation it is firm and is gritty like “when cutting an unripe pear” when transected. The specimen oftentimes contains DCIS . Infiltrating ductal carcinoma metastasizes to regional lymphnodes in the axilla and then to bones, lungs , liver and brain.
-
Infiltrating lobular carcinoma is seen in 5-10% of cases. Multicentricity and bilaterality are common. Microscopically it is famous for its cells arranged in Indian files. It metastasizes to axillary lymphnodes, and to unusual sites such as the meninges, and other serosal surfaces.
-
Tubular Carcinoma: (2% of cancers) . The diagnosis can only bemade when more than 75% of the tumor demonstrates tubular , well-formed glands. Axillary node metastases are unusual and this tumor has the best prognosis for any breast carcinoma with very low mortality.
-
Medullary Carcinoma: (5-7% of cancers). Microscpically it’s characterized by intense infiltration of lymphocytes and plasma cells and by the presence of a syncytial growth pattern, with little or no DCIS. This type of cancer is overrepresented in women with mutated BRCA-1 syndrome.
-
Mucinous or Colloid Carcinoma: (3%). Grossly, the tumor is a gelatinous mass. Microscopically lakes of mucin surround clumps of cells. It’s a slow growing tumor and prognosis tends to be favorable
Other types of breast malignancy include papillary, apoocrine, spindle cell carcinomas, and squamous cell carcinomas.
Diagnosis
Clinical presentation has changed significantly with the advent of mammography. In the past 55%-75% of breast cancers were diagnosed by self-examination, but currently mammographic screening programs have determined an increase in the identification of cancers that are non palpable and clinically occult.
Evaluation of the patient with potential breast cancer involves a multistep process that includes history, physical exam, ( routine breast self-examination remains an important diagnostic screening modality) and radiologic studies. Further investigations ( genetic analysis and biopsies) are guided by the findings within the three steps described above.
It is important the physical examination by complete: it should start with visual inspection ( peau d’orange, nipple inversion, erythema, asymmetry, masses, nipple changes), followed by examination in the sitting position including palpation of the breasts, axillary and supraclavicular lymphnode stations and the tail of the breast which is oftentimes overlooked). Palpation of the breast parenchyma is done with the patient in the supine position with the ipsilateral arm placed over the head. Additional evaluation in warranted for any palpable lesion in patients over 30 years of age seeing as physical exam cannot adequately differentiate between malignant and benign lesions( 20-40% error rate even among expert examiners)
Evaluation of a palpable lesion
Such evaluation should be undertaken based on the individual characteristics of each patient
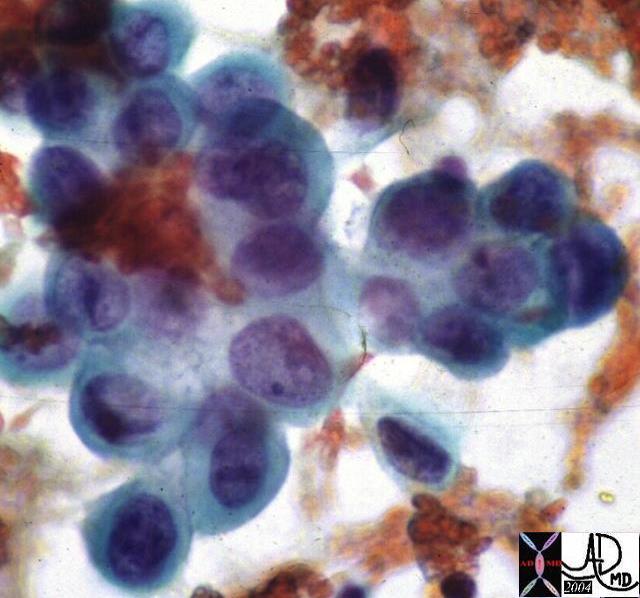
1) Mammography is usually the first step in this evaluation and serves two purposes. This is less accurate in youn patients with dense breast tissue and rarely used in patients under the age of 30( Ultrasound is used in such patients).
a) Assessment of the risk of malignancy of the mass (Calcifications, spiculation, nipple changes, axillary adenopathy)
b) Bilateral screening of non-palpable lesions
2) Fine needle aspiration (FNA) or core needle biopsy is usually the next step of the evaluation. Some advocate needle aspiration prior to mammographic evaluation, but a needle-puncture hematoma may confuse radiologic evaluation, and therefore mammography should precede biopsy.FNA is done with a 22 gauge needle and allows for differentiation between cystic and solid masses and provides a specimen for cytology.Oftentimes aspiration is curative for cystic lesions. Bloody cyst aspirate may be indicative of malignancy and should therefore always be sent for cytology (1% incidence of malignancy within breast cysts). Recurrent or complex (loculated ) cysts also have a greater incidence of malignancy. FNA provides material for cytologic evaluation of solid lesions. Once aspirated , the material is immediately fixed in 95% ethanol and sent to pathology. FNA , unlike core – needle biopsy- does not allow differentiation between in situ and invasive carcinoma.
Mammography represents the main diagnostic modality for non-palpable lesions
Mammographic signs of cancer can be divided in two main classes: density changes and microcalcifications
The American College of Radiology (ACR) is the copyright owner of a work entitled Breast Imaging Reporting and Data System (BI-RADS), which contains a guide to standardized mammographic reporting, including a breast-imaging lexicon of terminology, a report organization and assessment structure and coding system
Category 0: Need Additional Imaging Evaluation
Category 1: Negative
Category 2: Benign Finding
Category 3: Probably Benign Finding ? Short Interval Follow-Up Suggested
Category 4: Suspicious Abnormality ? Biopsy Should Be Considered
Category 5: Highly Suggestive of Malignancy ? Appropriate Action Should Be Taken
Suspicious lesions mandate further evaluation. US – guided biopsy is not useful in the evaluation of microcalcifications seeing as these are not visible sonographically. Stereotactic needle biopsy is useful in the evaluation of non-palpable lesions with microcalcifications
Imaging
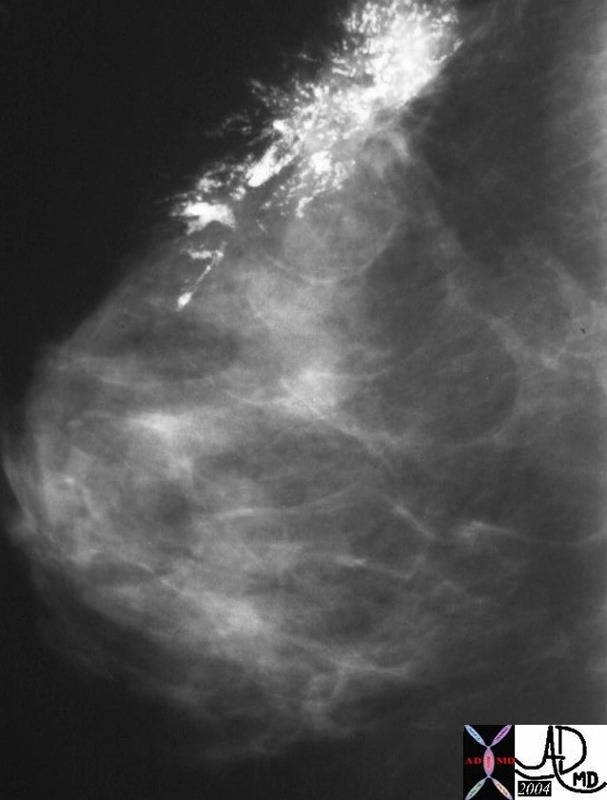
27975 breast hx 27F left breast lump fx pleomorphic calcification Rx lumpectomy dx intraductal carcinoma with high grade DCIS lymph node positive mammogram mammography Courtesy Priscilla Slanetz MD
Breast Cancer Survival Rate by Stage
Health care professionals are able to be predict a patient’s survival rate based on the determined stage of breast cancer. The following chart is an approximate survival rate for each stage of breast cancer. Percentages will vary depending on individual medical situations, etc.
Stage
|
5-year Relative
Survival Rate
|
0
|
100%
|
I
|
98%
|
IIA
|
88%
|
IIB
|
76%
|
IIIA
|
56%
|
IIIB
|
49%
|
IV
|
16%
|
Source: American Cancer Society
A five-year survival rate refers to the average number of patients who are still alive five years after diagnosis with a specific stage of breast cancer. After seven years, the survival rate decreases for each stage. The average Stage I breast cancer survival rate is 92%. The Stage II survival rate is 71%, Stage III survival rate is 39%, and the Stage IV survival rate is 11%.
It is important to remember that these survival rates are based on averages. Some women with advanced breast cancer live significantly longer than seven years. Researchers are constantly developing new treatment alternatives to prolong breast cancer survival.
Chemotherapy
CThe histologic status of the axilla, age of the patient, size of the primary tumor and extrogen/proesterone receptor status determine whether or not the patient will receive chemotherapy as an adjuvant or neoadjuvant therapy. Further factors that are considered include tumor pathologic characteristics ( ploidy, S-phase fraction, c-erbB-2 oncogine amplification, cathepsin D status) and the general health of the patient.
Multidrug chemotherapeutic regimens appear to significantly reduce the risk of recurrence and death in both lymphnode positive and lymphnode negative patients. The most frequently used regimen includes cyclophosphamide, methotrexate and 5-fluorouracil (4-8 weeks). The indications to the use fo tamoxifen are currently being broadened ( originally indicated for post-menopausal women with estrogen receptor-positive breast cancer) The use of tamoxifen for 5 years ( independent of age / menopausal status) is associated with a 47% reduction in the risk of breast cancer recurrence and a 26% reduction in the risk of death. Tamoxifen therapy has the added benefit of decreasing morbidity and mortality relate to cardiovascular disease, of increasing bone density and lowering cholesterol . Complications related to the use of such medication include an increase in the risk of thromboembolic disease and endometrial cancer.
Taxanes ( paclitaxel and docetaxel) represent a class of drugs that works by stabilizing the polymerization of microtubules, therefore arresting the cell cycle in the G2/M phase. They result in lack of resistance with other classes of drugs and have been used in crossover protocols for patients with anthracycline resistant tumors.
Trastuzumab (Herceptin) is a monoclonal antibody against the HER-2 / neu gene which codes for a Tyrosine Kinase that is overexpressed in 25% of breast cancers. Trials are currently looking at its efficacy in multidrug combination regimens.
Radiation Therapy
Radiation theraby can be delivered in the form of External beam radiation, Internal beam radiation, and intra-operative radiation. Radiation therapy is typically initiated 2-3 weeks after surgery or at the completion of postoperative chemotherapy. Daily outpatient radiation treatment lasts 5 o 6 weeks.
Prognosis
Numerous factors influence the prognosis of patients with breast cancer. The graphic representation below lists the factors associated with a poor prognosis
Breast Cancer Survival Rate by StagePatient’s survival rates are usually determined based on the stage of breast cancer.
Staging Breast Cancer
|
Stage
|
Tumor Size
|
Lymph Node Involvement
|
Metastasis (Spread)
|
I
II
III
IV
|
Less than 2 cm
Between 2-5 cm
More than 5 cm
Not applicable
|
No
No or in same side of breast
Yes, on same side of breast
Not applicable
|
No
No
No
|
Stage
|
5-year Relative
Survival Rate
|
0
|
100%
|
I
|
98%
|
IIA
|
88%
|
IIB
|
76%
|
IIIA
|
56%
|
IIIB
|
49%
|
IV
|
16%
|
Source: American Cancer Society
A five-year survival rates represent the average number of patients who are still alive five years after diagnosis with a specific stage of breast cancer.These survival rates are based on averages and are subject to significant variability between individuals.
Interesting Facts

Tiepolo, Giambattista The Martyrdom of Saint Agatha c. 1755 Gemaeldegalerie, Staatliche Museen Preussischer Kulturbesitz, Berlin
 Photograph courtesy of the Kunsthistorisches Institut Florenz, Florence, Italy Photograph courtesy of the Kunsthistorisches Institut Florenz, Florence, Italy
|

 Photograph courtesy of the Kunsthistorisches Institut Florenz, Florence, Italy
Photograph courtesy of the Kunsthistorisches Institut Florenz, Florence, Italy